克罗恩病是银屑病及银屑病关节炎的因果风险因素
- ①纳入463372名欧洲人,包括12882例IBD患者、5621例银屑病患者、2063例银屑病关节炎患者;
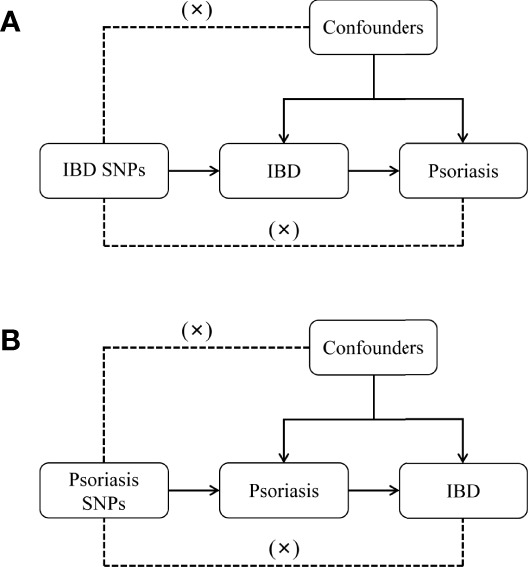
- ②单变量孟德尔随机化(MR)分析表明,基于遗传因素预测的IBD与较高的银屑病和银屑病关节炎的风险显著相关;
- ③多变量MR分析表明,基于遗传因素预测的克罗恩病(而非溃疡性结肠炎)与较高的银屑病及银屑病关节炎的风险显著相关;
- ④基于遗传因素预测的银屑病或银屑病关节炎与IBD(包括克罗恩病及溃疡性结肠炎)风险无显著关联。
- JAMA Dermatology上发表的一项孟德尔随机化研究结果,对超过46万名欧洲人的数据进行分析后发现,IBD(尤其是克罗恩病)是银屑病及银屑病关节炎的因果风险因素,但反之的因果关联则不成立。
IBD与银屑病及银屑病关节炎之间的关联:双向双样本孟德尔随机化研究
10.1001/jamadermatol.2022.3682IF: 10.9 Q1
2022-09-14, Article
Abstract:收起
Importance: Psoriasis, psoriatic arthritis, and inflammatory bowel disease, ie, Crohn disease and ulcerative colitis, are chronic systemic immune-mediated disorders affecting an increasing proportion of adults and children worldwide. Observational studies have suggested an association between inflammatory bowel disease and psoriasis and vice versa. So far, however, it remains unclear whether and in which direction causal relationships exist.
Objective: To investigate the association between inflammatory bowel disease, particularly Crohn disease and ulcerative colitis, and psoriasis or psoriatic arthritis.
Design, Setting, and Participants: A bidirectional 2-sample mendelian randomization study was conducted using summary statistics from genome-wide association studies including up to 463 372 European individuals. Total and direct effects were derived performing an iterative radial and robust inverse-variance weighted method within the univariable and multivariable mendelian randomization setting, respectively. Causal estimates were verified using a validation inflammatory bowel disease sample, a series of pleiotropy-robust mendelian randomization methods, and sensitivity analyses based on a PhenoScanner search in conjunction with network analysis. Data analysis was performed from April to May 2022.
Main Outcomes and Measures: Inflammatory bowel disease, Crohn disease, ulcerative colitis, psoriasis, and psoriatic arthritis were used as both exposures and outcomes.
Results: The European samples included 12 882 cases of inflammatory bowel disease and 5621 cases of psoriasis. The proportion of women ranged between 48% and 56%. Genetically predicted inflammatory bowel disease was associated with higher risk of psoriasis (pooled odds ratio [OR], 1.10; 95% CI, 1.05-1.15; P < .001) and psoriatic arthritis (pooled OR, 1.10; 95% CI, 1.04-1.18; P = .003). In contrast with ulcerative colitis, the Crohn disease subentity was associated with psoriasis (OR, 1.16; 95% CI, 1.12-1.20; P < .001) and psoriatic arthritis (OR, 1.13; 95% CI, 1.06-1.20; P < .001). Regarding the reverse directions, no notable associations could be found.
Conclusions and Relevance: Findings of this mendelian randomization study support a causal effect between inflammatory bowel disease and psoriasis as well as psoriatic arthritis, but not vice versa. It seems that especially Crohn disease and not ulcerative colitis is responsible for the causal effect of inflammatory bowel disease on both psoriasis outcomes. These findings have implications for the management of inflammatory bowel disease and psoriasis in clinical practice.
First Authors:
Dennis Freuer
Correspondence Authors:
Dennis Freuer
All Authors:
Dennis Freuer,Jakob Linseisen,Christa Meisinger
Li Y, Guo J, Cao Z, Wu J. Causal Association Between Inflammatory Bowel Disease and Psoriasis: A Two-Sample Bidirectional Mendelian Randomization Study. Front Immunol. 2022 Jun 10;13:916645. doi: 10.3389/fimmu.2022.916645IF: 7.3 Q1 . PMID: 35757704; PMCID: PMC9226443.
推荐:
Causal effect identified for inflammatory bowel disease with psoriasis, psoriatic arthritis